Differential diagnosis of bowel diseases can be challenging, because most of them present with similar common symptoms: abdominal pain and discomfort, diarrhea, weight loss. Infections by common gastrointestinal pathogens may soon be identified, but discrimination of inflammatory bowel disease, of which ulcerative colitis and Crohn’s disease are the most common, and irritable bowel syndrome, remains difficult.
Differential diagnosis of bowel diseases can be challenging, because most of them present with similar common symptoms: abdominal pain and discomfort, diarrhea, weight loss. Infections by common gastrointestinal pathogens may soon be identified, but discrimination of inflammatory bowel disease, of which ulcerative colitis and Crohn’s disease are the most common, and irritable bowel syndrome, remains difficult.
Inflammatory bowel disease (IBD) is characterised by inflammation of the bowel, which is not seen in most patients with irritable bowel syndrome (IBS), and both conditions request different diagnostic and therapeutic approaches. IBD are serious diseases with severe comorbidities, and affected patients need further investigation with extensive diagnostic measures and intensive medical treatment. In contrast to that, IBS may be painful and impairs quality of life, but it does not usually cause serious morbidity. However, patients with IBS can have symptoms for many years and they often experience unnecessary and stressing diagnostic procedures.
Several studies have documented that testing for calprotectin in stool samples of affected patients may help to avoid unnecessary invasive diagnostic tests in people with irritable bowel syndrome and contribute to faster identification of patients suffering from inflammatory bowel disease who need intensive specialist care.
These findings have led to the development of a new guideline on fecal calprotectin diagnostic tests for inflammatory diseases of the bowel, issued by the british National Institute for Heath and Care Excellence (NICE) in October 2013: NICE diagnostics guidance 11, October 2013; Faecal calprotectin diagnostic tests for inflammatory diseases of the bowel
Lower bowel symptoms are very common in general practice. In most cases they are associated with irritable bowel syndrome. However, the symptoms can be caused by inflammatory bowel disease, which can lead to serious complications. Inflammatory bowel diseases (IBD) and irritable bowel syndrome (IBS) are presenting with similar symptoms, but they are totally different diseases. It is therefore important to distinguish IBD from IBS, so that each of the conditions can be appropriately managed and monitored. Patients with IBD need to be referred to a gastroenterology specialist for further investigation, who confirms the diagnosis of IBD by clinical evaluation and a combination of biochemical, endoscopic, radiological, histological, or nuclear medicine based examinations.
Initial laboratory investigations in common practice include full blood count, erythrocyte sedimentation rate, C-reactive protein and other tests. Erythrocyte sedimentation rate and C-reactive protein are the main markers used to measure intestinal inflammation. However, these tests can be influenced by non-intestinal diseases and can lack diagnostic accuracy. Moreover, while both tests indicate inflammation, they cannot localise it to the bowel. As a result, many IBS patients are referred for further invasive diagnostic tests involving endoscopy, which may not be needed.
According to the new NICE diagnostics guidance:
“Faecal calprotectin is accurate in detecting colonic inflammation and concentration of faecal calprotectin correlates with the level of bowel inflammation. Therefore, determination fecal calprotectin contributes to identification of functional diarrhea and helps to avoid unnecessary endoscopies and biopsies.”
Calprotectin
Calprotectin is a calcium- and zinc-binding protein that has antimicrobial properties and is ubiquitous throughout the body. The cytoplasm of polymorphonuclear granulocytes contains up to 60 % calprotectin. It is also found in trace concentrations in monocytes and macrophages.

The faecal calprotectin level is a measure of inflammation-induced migration of granulocytes into the intestinal lumen and correlates directly with the intensity of the inflammatory reaction of the intestinal mucosa. Elevated levels of calprotectin in stool samples are found in patients with IBD, infectious gastroenteritis, necrotizing enterocolitis, allergic colitis, cystic fibrosis or colorectal carcinoma. Patients with celiac disease or with functional disorders like IBS have normal values of faecal calprotectin.
The detection of faecal calprotectin is a simple, non-invasive test that can reasonably be carried out before any imaging or endoscopy. Calprotectin in stool is a sensitive marker for inflammatory bowel disease and is particularly useful for differentiating irritable bowel syndrome. In addition, measurement of calprotectin level facilitates evaluation of disease activity in chronic inflammatory bowel disease and thus also aids in monitoring progression of the disease and its treatment.
According to the NICE guidance, calprotectin test results need to be interpreted in the context of a cut-off value, below which the test is deemed negative and above which it is deemed positive.
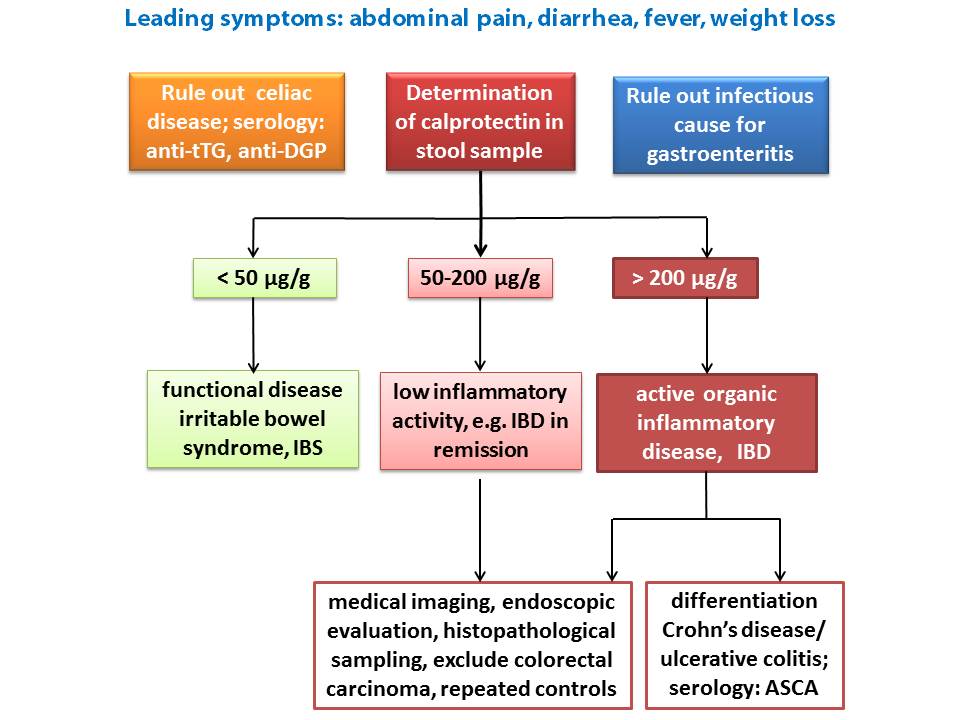
A test result in the normal range (below 50 µg calprotectin / g stool) would support a diagnosis of IBS, a disease not characterised by inflammation.
A middle range is defined, where calprotectin levels are only slightly elevated, for classification of inflammation and monitoring of disease activity. A test result in the middle range, where calprotectin concentrations are slightly elevated, indicates a low level of inflammatory activity in the gastrointestinal tract. Repeated tests and further diagnostic measures are recommended.
Significantly elevated levels of calprotectin ( > 200 µg/g) are associated with active organic bowel disease and further intensive diagnostic tests and treatment by a specialised gastroenterologist are urgently advised.
Irritable Bowel Syndrome, IBS
IBS is a functional bowel disorder characterised by frequent bouts of bowel disturbance, abdominal pain and discomfort, and bloating. It may occur related to prior infection with gastrointestinal pathogens, but a clear cause has not yet been identified, no distinctive pathology is known and treatment is symptomatic. Dietary factors or stress may trigger exacerbations. Physiological studies often show an increase in bowel sensitivity, and the condition may be associated with abnormal muscle activity in the wall of the bowel. IBS can be painful, disrupt normal activities and reduce quality of life because of disturbed work and sleep, and anxiety. Symptoms of IBS can last for many years. It is troublesome , although it does not usually cause serious morbidity.
The NICE clinical guideline on irritable bowel syndrome in adults suggests a prevalence of between 10% and 20% in the general population. The true prevalence of IBS may be higher than estimated because many people with IBS symptoms do not seek medical advice. IBS most commonly affects people between the ages of 20 and 30 years and it is twice as common in women as in men. Recent evidence shows that there is also a significant prevalence of IBS in older people. The percentage of people with IBS is greater in adults than in children. Patients that meet the IBS diagnostic criteria should receive further laboratory tests to exclude other diagnoses, e.g. full blood count, erythrocyte sedimentation rate or plasma viscosity, C-reactive protein, and antibody testing for coeliac disease (anti-tissue transglutaminase antibody, anti-DGP or anti-endomysial antibodies). For more information see related blog post on celiac disaese diagnostics.
Distinction of irritable bowel syndrome from inflammatory bowel disease on clinical grounds alone is not always possible. Therefore, colonoscopy in specialist care is often performed to confirm the final diagnosis, an invasive and unpleasant procedure. Testing for calprotectin in stool samples is a non-invasive, reliable and simple method to detect intestinal inflammation. A negative test result for calprotectin supports the diagnosis of IBS as a non-inflammatory cause for the symptoms. When calprotectin measurements indicate a probably inflammatory cause of the symptoms, the next level of investigation should involve endoscopy and imaging.
The picture below illustrates a possible diagnostic algorithm for discrimination of IBS and IBD with non-invasive serologic tests:
Inflammatory Bowel diseases, IBD
IBD, such as Crohn’s disease and ulcerative colitis are autoimmune conditions that involve inflammation of the gastrointestinal tract. These diseases can have serious complications, including a high risk of surgery. In both, ulcerative colitis and Crohn’s disease, some people have active disease but no symptoms. Typically, the diseases have a relapsing–remitting pattern with seemingly healthy, asymptomatic periods alternating with phases of severe inflammation.
Ulcerative colitis is the most common type of inflammatory disease of the bowel. It has an incidence in the UK of approximately 10 per 100,000 people annually, and a prevalence of approximately 240 per 100,000. This amounts to around 146,000 people in the UK with a diagnosis of ulcerative colitis.
The cause of ulcerative colitis is unknown. A genetic predisposition exists and smoking is a triggering factor. The disease can develop at any age, but peak incidence is between the ages of 15 and 25 years, with a second, smaller peak between 55 and 65 years. Ulcerative colitis usually affects the rectum, and a variable extent of the colon proximal to the rectum. The inflammation is continuous in extent. Inflammation of the rectum is referred to as proctitis, and inflammation of the rectum and sigmoid as proctosigmoiditis. Left-sided colitis refers to disease involving the colon distal to the splenic flexure. Extensive colitis affects the colon proximal to the splenic flexure, and includes pancolitis, where the whole colon is involved. For more information on management of ulcerative colitis refer to the NICE guideline ulcerative colitis, issued in June 2013. A fast, easy summary view of NICE guidance on ‘ulcerative colitis’ is given in the NICE pathway ulcerative colitis .
Prognosis of Crohn’s disease is worse than prognosis of ulcerative colitis. Only 10% of people with this condition vs. 50 % of patients with ulcerative colitis have prolonged remission. In about 20% of patients with ulcerative colitis and 50 % of patients with Crohn’s the disease will be chronic and 10 years after onset, 20–30% of patients with ulcerative colitis and 50 % of those with Crohns disease will have needed surgical removal of the colon. Life expectancy is slightly decreased in people with Crohn’s disease compared to the general population and constant surveillance for colorectal cancer is needed. In 2012 NICE has published the clinical guideline Crohn’s disease: management in adults children and young people, summerised in a corresponing Crohn’s disease pathway.
Crohn’s disease and ulcerative colitis are chronic diseases that are associated with significant morbidity. They affect a person’s social and psychological wellbeing, particularly if they are poorly controlled. Patients affected with these inflammatory diseases need life-long intensive medical treatment. The invention of new biologic medications, such as anti-tumour necrosis factor, has offered the possibility to achieve mucosal healing, maintain remission and improve patients’ quality of life.
Calprotectin is a simple and established non-invasive laboratory parameter, and determination of calprotectin in stool samples will be beneficial for distinguishing patients with inflammatory bowel diseases or irritable bowel syndrome already on the level of primary care. Patients with suspected severe inflammatory disease can be referred quickly to specialist care for further investigation by clinical evaluation and a combination of biochemical, endoscopic, radiological, histological, or nuclear medicine based examinations. Tests for faecal calprotectin distinguish non-inflammatory irritable bowel syndrome from inflammatory bowel diseases and support the detection of inflammatory bowel disease even before clinical symptoms occur. Moreover, calprotectin levels correspond to disease activity, making the calprotectin tests an ideal tool for monitoring response to therapy in IBD and for early detection of relapses.
Further reading
- Burri E and Beglinger C, Faecal calprotectin — a useful tool in the management of inflammatory bowel disease. Swiss Med Wkly 2012. 142: w13557. => Link to full text article
- Canani RB, Terrin G, Rapacciuolo L, Miele E, Siani MC, Puzone C, Cosenza L, Staiano A, Troncone R. Faecal calprotectin as reliable non-invasive marker to assess the severity of mucosal inflammation in children with inflammatory bowel disease. Dig Liver Dis 2008; 40: 547-53. => Link to article abstract
- D’Haens G, Ferrante M, Vermeire S, Baert F, Noman M, Moortgat L, Geens P, Iwens D, Aerden I, Van Assche G, Van Olmen G, Rutgeerts P. Fecal calprotectin is a surrogate marker for endoscopic lesions in inflammatory bowel disease. Inflamm Bowel Dis 2012; 18: 2218-24. => Link to article abstract
- Dubinsky, M. C., Ofman, J. J., Urman, M., Targan, S. R., and Seidman, E. G., Clinical utility of serodiagnostic testing in suspected pediatric inflammatory bowel disease. Am J Gastroenterol 2001; 96: 758-765. => Link to article abstract
- Dubinsky M .C., Serologic and laboratory markers in prediction of the disease course in inflammatory bowel disease. World J Gastroenterol; 2010; 16: 2604-2608. => Link to full text article
- Gisbert JP, McNicholl AG. Questions and answers on the role of faecal calprotectin as a biological marker in inflammatory bowel disease. Dig Liver Dis. 2009; 41: 56-66. =>Link to article abstrract
- Kostakis ID, Cholidou KG, Vaiopoulos AG, Vlachos IS, Perrea D, Vaos G. Fecal calprotectin in pediatric inflammatory bowel disease: a systematic review. Dig Dis Sci. 2013; 58: 309-19. =>Link to article abstract
- Manz M., Burri E., Rothen C., Tchanguizi N., Niederberger ,C., Rossi, L., Beglinger, C., and Lehmann, F. S., Value of fecal calprotectin in the evaluation of patients with abdominal discomfort: an observational study. BMC. Gastroenterol. 2012; 12: 5. => Link to full text article
- Smith LA, Gaya DR. Utility of faecal calprotectin analysis in adult inflammatory bowel disease. World J Gastroenterol. 2012 Dec 14;18(46):6782-9. doi: 10.3748/wjg.v18.i46.6782. => Link to full text article
[/pc-pvt-content]